What is your Gut Feeling?
Have you ever paid attention to what your Gut is telling you? (P.S: it is usually the truth!)
After all these years of hearing the advice to follow your Gut instinct, there is abundant emerging scientific proof that it might be wise to heed that advice!
The average human body is inhabited by at least 10 times more bacteria than the number of human cells in the body, for a total of about 1000 more genes than are present in the human genome.
The human Microbiome is the collection of all the microorganisms living in association with the human body. These communities consist of a variety of microorganisms including eukaryotes, archaea, bacteria and viruses. the majority of those bacteria are found in the human gastrointestinal tract (1). They make up only about 1 to 3 percent of our body mass due to their minuscule size(that’s 2 to 6 pounds of bacteria in a 200-pound adult).
This is a wonderful video to learn more about the invisible Human Microbiome
The concept of the human Microbiome was first suggested by Joshua Lederberg, who coined the term “Microbiome” to signify “the ecological community of commensal, symbiotic, and pathogenic microorganisms that literally share our body space” (2).
We are essentially a very complex and interconnected ecosystem containing trillions of bacteria and other microorganisms that inhabit all our surfaces; including our skin and mucosal surfaces like mouth, sexual organs, and specially the gut. There are over 100 trillion microbes that frolic in our gut, constituting our “Second Brain”.
It has recently become evident that the Gut microbiota can strongly influence many physiological parameters, including cognitive functions, such as learning, memory and decision making processes. Since about 2005, scientists have begun to understand the 2 way communication relationship between the digestive process and brain function and development. This is called the gut-brain axis.
How Does it Work?
Gut Flora benefit the host by multiple mechanisms like: processing the energy from the fermentation of undigested carbohydrates and the subsequent absorption of short-chain fatty acids, like Butyrates, Propionates and acetates; synthesizing vitamin B and vitamin K; producing helpful anti-inflammatory compounds that fight off other disease-causing microbes; metabolizing bile acids, sterols, and xenobiotics; and playing a major role in immune function. Gut bacteria also produce hundreds of neuro-chemicals that the brain uses to regulate basic physiological processes as well as mental processes such as learning, memory and mood.
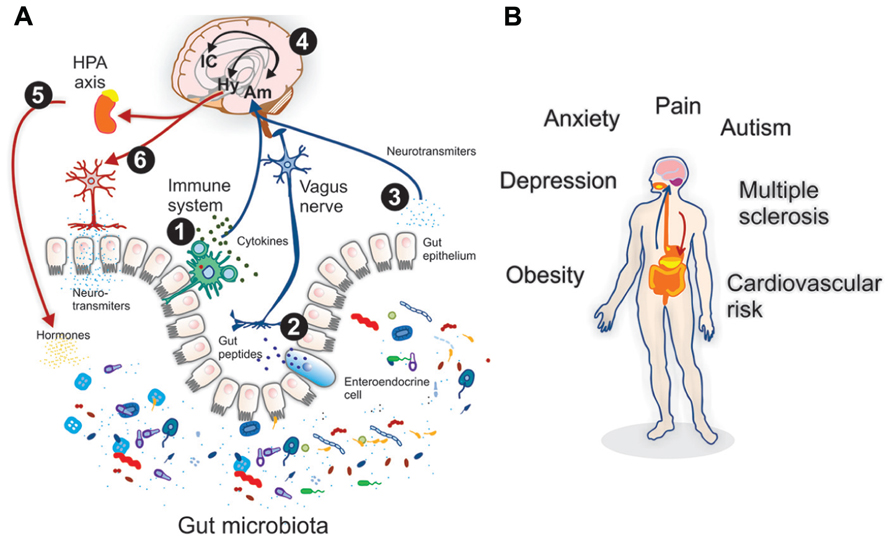
The Gut communicates with the central nervous system through different pathways (neural, immune and endocrine) and influences the brain. For example, gut bacteria manufacture about 95 percent of the body’s supply of serotonin, which influences both mood and GI activity.
The metabolic activities performed by these bacteria resemble those of an organ, leading some to liken gut bacteria to a “forgotten” organ. (3)
It’s All About You (no, really.)
Two thirds of the gut Microbiome is unique to each individual. Most of these microbes are essential for maintaining health. An ever-growing number of studies have demonstrated that changes or Imbalance in the composition of our Microbiome, called Dysbiosis, correlate with numerous disease states, raising the possibility that manipulation of these communities could be used to treat disease. Dysbiosis can be a result of excessive antibiotic use, alcohol misuse or inappropriate diet.
Recent and growing evidence suggests that several health conditions may be affected by intestinal microbiota, including: visceral pain, autism spectrum disorders , obesity , cardiovascular risk, anxiety/depression, Irritable Bowel Syndrome, Inflammatory bowel disease, SIBO (Small intestinal bacterial Overgrowth), bacterial vaginosis, and multiple sclerosis. (4)
The Gut Microbiome and the Brain
The human gut Microbiome impacts human brain health in numerous ways including stimulation of the innate immune system, can produce systemic and/or central nervous system inflammation, stimulate dysfunctional responses of the adaptive immune system, may produce neurotoxic metabolites , produce hormones and neurotransmitters , stimulate afferent neurons of the enteric nervous system to send signals to the brain via the vagus nerve.
Through these varied mechanisms, gut microbes shape the architecture of sleep and stress reactivity of the hypothalamic-pituitary-adrenal axis. They influence memory, mood, and cognition and are clinically and therapeutically relevant to a range of disorders, including alcoholism, chronic fatigue syndrome, fibromyalgia, and restless legs syndrome. Their role in multiple sclerosis and the neurologic manifestations of celiac disease is being studied. Nutritional tools for altering the gut Microbiome therapeutically include changes in diet, probiotics, and prebiotics.
Several studies have shown that the gut microbiota is involved in the regulation of anxiety, pain, cognition and mood. These studies used germ free animals (GF) compared to normal animals or specific pathogen free (SPF), which were later exposed to pathogenic bacterial infections, probiotic bacteria and antibiotic drugs.
It is now evident that the bidirectional signaling between the gastrointestinal tract and the brain, mainly through the vagus nerve, the so called “microbiota–gut–vagus–brain axis,” is vital for maintaining homeostasis and it may be also involved in the etiology of several metabolic and mental dysfunctions/disorders. (5) (6)
Evidence suggests modulation of neuro-immunologic, neuro-inflammatory, and neuro-hormonal pathways. Other mechanisms identified include modulation of the hypothalamic–pituitary–adrenal axis, the vagus nerve, microglia, myelination, and prefrontal cortex gene expression.
Researchers found noticeable improvements in the ability of rats to cope with stressful activity (such as swimming) when diets are supplemented by specific gut microbiota.
The mice showed increased motor activity and reduced anxiety. elevated levels of neurotransmitters like noradrenaline, dopamine, and 5-hydroxytryptamine turnover in the striatum , which is involved in a number of different cognitive processes.
When SPF mice are exposed to antibiotics, gastrointestinal infections and stress, sharp changes in diet, the gut homeostasis and the central nervous system becomes imbalanced, suggesting a role for the gut microbiota in the regulation of anxiety, mood, cognition and pain.
Lactobacilli and Bifidobacteria can reduce visceral pain induced by stress and IBS, in humans and mice, and many different probiotics have been shown to have beneficial effects in humans with abdominal pain. Most probiotics modulate the immune system, decrease anxiety, and reduce the stress-induced increase of corticosterone to decrease stress. Other probiotics can lower inflammatory cytokines, decrease oxidative stress, and improve nutritional status. (7)(8)
Depression, Anxiety, Autism
Different Microbes are also implicated in depression. The pathogenic bacterium Borrelia burgdorferi causes Lyme disease which causes depression in up to 2/3 of all cases.(9)
Human patients with depression are less able to properly digest fructose, which is also associated with a reduction in tryptophan production.Eliminating fructose from their diet improved their depression. (10)
In humans, anxiety disorders are common in patients with disturbed gut flora. Autistic populations have a unique microbiome consisting of more clostridial species.
Since some of the microbes in the human body can also modify the regulation of some neurotransmitters, it may be possible to use certain microorganisms to supplement treatments for depression,bipolar disorder and other stress-related psychiatric disorders.(11)
The vagus nerve has been identified as a major modulatory constitutive communication pathway between the bacteria exposed to the gut and the brain. highlighting the important role of bacteria in the bidirectional communication of the gut–brain axis and suggested that certain organisms may prove to be useful therapeutic adjuncts in stress-related disorders such as anxiety and depression.
Studies of microbiota-gut-brain communication are providing us with a deeper understanding of the relationship between the gut bacteria and their hosts while also suggesting the potential for microbial-based therapeutic strategies that may aid in the treatment of mood disorders.
Other Connections
On communication between gut microbes and the brain.(12)
The human Microbiome may also have a role in auto-immune diseases like diabetes, rheumatoid arthritis, muscular dystrophy, multiple sclerosis, fibromyalgia, and even some cancers. (13)
A strategy to understand the microbial components of the human genetic and metabolic landscape and how they contribute to normal physiology and predisposition to disease has been taken up by The Human Microbiome project. (14)
Various treatments involving microbiota have been used in attempts to treat the dysbiosis and resulting illnesses, including Probiotics, prebiotics, synbiotics, Fecal microbiota transplantation (FMT), Dietary alterations etc. Diet could play a large role in helping to rebalance gut microbiota. Restricting unnecessary antibiotic exposure, limiting alcohol, managing stress well, and eating a healthy diet, will all help in the Healing process.
It might serve us well to be more mindful and listen to what our second brain tries to tell us on a day-to-day basis….we will be much healthier for listening!
Sources:
- Savage 1977
- Lederberg and McCray 2001
- O’Hara, A. M.; Shanahan, F. (2006). “The gut flora as a forgotten organ”. EMBO Reports 7 (7): 688–693.doi:10.1038/sj.embor.7400731. PMC 1500832. PMID 16819463.
- Leo Galland. http://www.adiitalia.net/documenti/dalla-letteratura/ThegutMicrobiome-30gennaio15.pdf
- Montiel-Castro, A. J. et al “The microbiota-gut-brain axis: Neurobehavioral correlates, health and sociality”.Frontiers in Integrative Neuroscience doi:10.3389/fnint.2013.00070.
- Crumeyrolle-Arias M, et al. Absence of the gut microbiota enhances anxiety-like behavior and neuroendocrine response to acute stress in rats. Psychoneuroendocrinology. 2014;42:207–17.CrossRefPubMed
- Mind-altering microorganisms: the impact of the gut microbiota on brain and behavior http://www.nature.com/nrn/journal/v13/n10/full/nrn3346.html
- The role of gut microbiota in the gut-brain axis: current challenges and perspective
http://link.springer.com/article/10.1007%2Fs13238-013-3017-x - Fallon, B. A.; Nields, J. A. (1994). “Lyme disease: A neuropsychiatric illness”.The American Journal of Psychiatry 151(11): 1571–1583.doi:10.1176/ajp.151.11.1571. PMID 7943444.
- Ledochowski, M.et al. “Fructose- and sorbitol-reduced diet improves mood and gastrointestinal disturbances in fructose malabsorbers”. Scandinavian journal of gastroenterology 35 (10): 1048–1052. doi:10.1080/003655200451162. PMID 11099057
- Bravo, Javier A.; et al. (2011). “Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve”.Proceedings of the National Academy of Sciences 108 (38): 16050–16055.doi:10.1073/pnas.1102999108. PMC: 3179073. PMID 21876150.
- http://www.ncbi.nlm.nih.gov/pubmed/?term=23010679
- Systemic effects of gut microbiota and its relationship with disease and modulation
http://link.springer.com/article/10.1186/s12865-015-0083-2#Sec1 - “The Human Microbiome Project”. Nature 449: 804–810. doi:10.1038/nature06244.
PMID 17943116.



